What tests could potentially be used for the screening, diagnosis and monitoring of COVID-19 and what are their advantages and disadvantages?
BACKGROUND
A range of molecular techniques ranging from central laboratory testing to point-of-care tests are under development or already available for the diagnosis and management of COVID-19 patients. These techniques, while well-known to researchers and clinicians with a background in deoxyribonucleic acid (DNA) amplification, as well as antibody and antigen assays, may be relatively unknown to the broader community. This document was written to outline and explain the basic principles of the main COVID-19 diagnostic tests currently in use or in trials.
Antibody – Antibodies are protective proteins produced naturally in response to seeing foreign structures (antigens), e.g. during a viral infection. The body produces early `prototype’ antibodies (IgM) with intermediate strength for binding to the virus. These are able to start working to clear virus about five days after a new infection started. Typically eight to ten days after the start of the infection, IgG antibodies with high binding strength, can work to help more rapid virus clearance. Antibodies act by developing a matching contoured surface to stick to antigens, using a sophisticated selection process to amplify antibodies with the best surface match and strongest binding.
Antigen – An antigen is a structure recognised as foreign by the human body that triggers the immune system to produce self defence systems to clear pathogens from blood and tissues. Antigen clearance is spearheaded by antibodies and white blood cells.
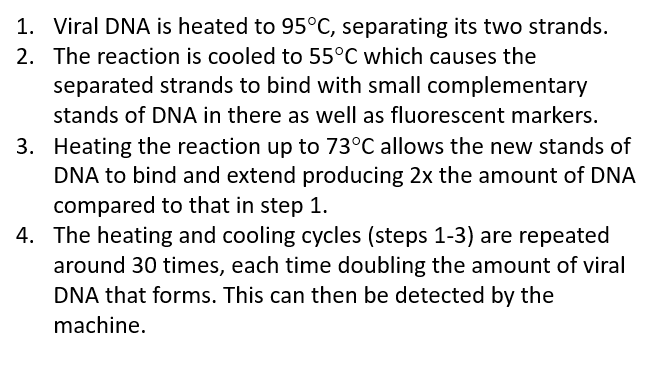
COVID-19 – Coronavirus disease-19 – A respiratory illness caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), colloquially referred to as coronavirus. The family of coronaviruses includes not only SARS (-1 and -2) and MERS, but also milder forms (causing 15-20% of common colds).
DNA – Deoxyribonucleic acid – The molecule that humans and most organisms use to store their genetic code. DNA contains the information that cells use to make proteins. It is formed from two strands that bind together forming a helix shape.
Enzyme – An enzyme is a protein that speeds up chemical reactions by adapting or changing other proteins and molecules.
Fluorescence – This is the light given off by certain molecules when they absorb energy.
Herd-Immunity – This method of protection from the spread of disease provides population immunity by vaccinating a large percentage of the population, thereby protecting those who are not immune by reducing their chance of exposure to the disease.
RNA – Ribonucleic acid – In humans RNA has many functions, but a main one is to copy sentences of DNA to make proteins. Some viruses use RNA instead of DNA to store their genetic code, including the virus that causes COVID-19.
Sensitivity – The ability of a diagnostic test to give a positive result when it is supposed to be positive.
Serum – Serum is a yellowish fluid which is part of the blood. It is the liquid component of blood once the blood cells have been removed.
Specificity – The ability of a diagnostic test to indicate a negative result when it is supposed to be negative.
Swab – A small piece of gauze or other absorbent material attached to a stick used for collecting patient samples. Both long and short swabs are used in coronavirus testing. Long swabs are used by a clinician to take nasal swabs, but short swabs can be used by patients themselves. Different protocols may require different swab types.
Reverse-Transcription Polymerase Chain Reaction (RT-PCR)
Technology overview
PCR is a very common scientific technique that has been widely used in research and medicine for around 20-30 years to detect genetic information. RT-PCR is a special version used when RNA is being detected and it is now being used as a test to detect SARS-CoV-2, the virus causing COVID-19. This type of test has frequently been used as a frontline test for COVID-19 as it directly tests for the presence of the virus RNA.
RT-PCR tests are fairly quick, sensitive and reliable, capable of producing results in 3-4 hours, although this usually takes longer if samples must first be sent to specialised external laboratories (6-8 hours on average).
Many diagnostic and research companies produce RT-PCR products, tests and machines so the technology is widely available. Some RT-PCR tests are developed as an `all in one’ kit, reducing laboratory handling and potential for contamination.
How it works
Once a sample has been collected, chemicals are used to remove any proteins, fats and other molecules, leaving only RNA behind. This will be a mixture of a person’s genetic material as well as any viral RNA that might be present.
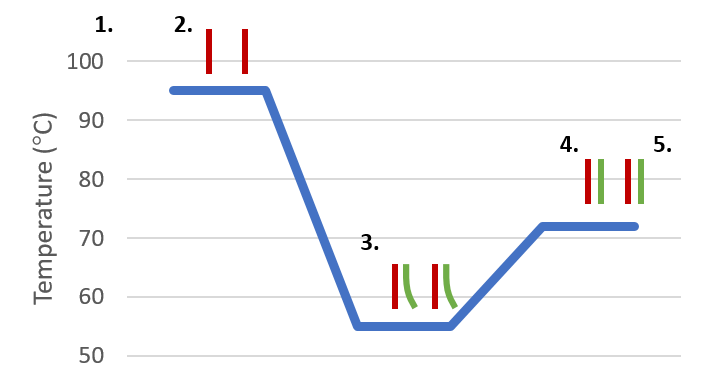
The test kit enzymes copy the RNA to DNA, which is amplified to allow virus detection by using a PCR machine which cycles the test temperature so that roughly 35 billion copies of viral DNA are made for each viral RNA strand that was originally present.
Fluorescent markers are typically used to bind to the amplified DNA and produce light, which can be read by the machine to produce the test result. If the intensity of the light produced within the sample reaches a certain threshold, this is classed as a positive test. The number of PCR temperature cycles that were required before the fluorescence threshold was reached is recorded and gives an estimate of how much virus was present in the patient sample.
Advantages and limitations
Advantages:
- RT-PCR is accepted by scientists and medical staff as a robust and well documented technique.
- With RT-PCR being so common in research and medicine, the technology is already in place to test for COVID-19.
- RT-PCR can detect current infections of disease, allowing medical staff to determine who is currently infected and who is not.
Disadvantages:
- RT-PCR relies on capturing and detecting the virus and so it is possible to miss patients who have cleared virus and recovered from disease.
- The distribution of virus across the respiratory tract varies between patients, so even if a person is infected, the virus may only be detectable in sputum or nasopharyngeal swab but not necessarily at both locations at the same time.
- RT-PCR for COVID-19 can only tell if a person is currently infected with this particular coronavirus. It can’t provide information on other diseases or symptoms.
